Chapter 3: Nutrients in the Body
3.7 Digestive Hormones, Accessory Organs, and Secretions
Before we go into the digestive details of specific macronutrients, it is important that you have a basic understanding of the anatomy and physiology of the following digestion accessory organs: pancreas, liver, and gallbladder. Digestion accessory organs assist in digestion, but are not part of the gastrointestinal tract. How are these organs involved?
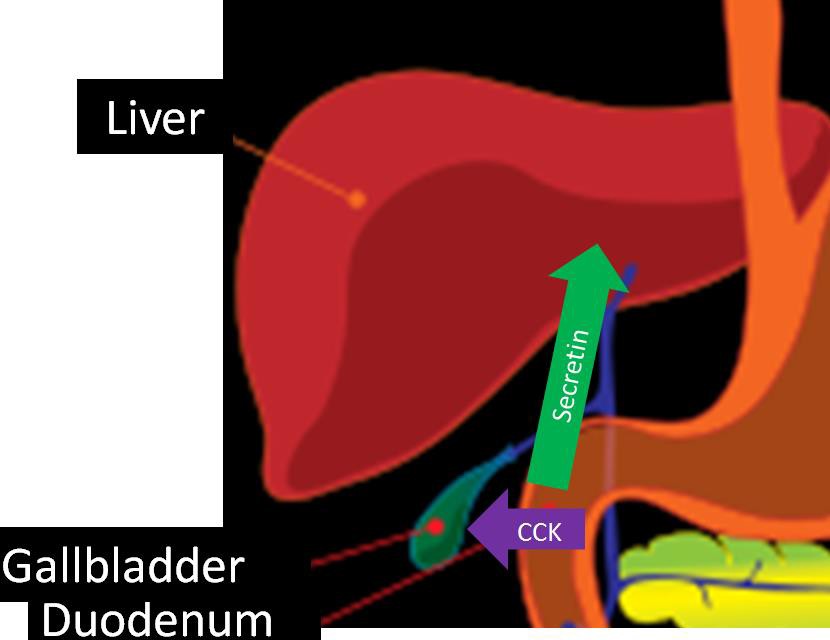
Upon entering the duodenum, the chyme causes the release of two hormones from the small intestine: secretin and cholecystokinin (CCK) in response to acid and fat, respectively. These hormones have multiple effects on different tissues. In the pancreas, secretin stimulates the secretion of bicarbonate (HCO3), while CCK stimulates the secretion of digestive enzymes. The bicarbonate and digestive enzymes released together are collectively known as pancreatic juice, which travels to the small intestine, as shown below.
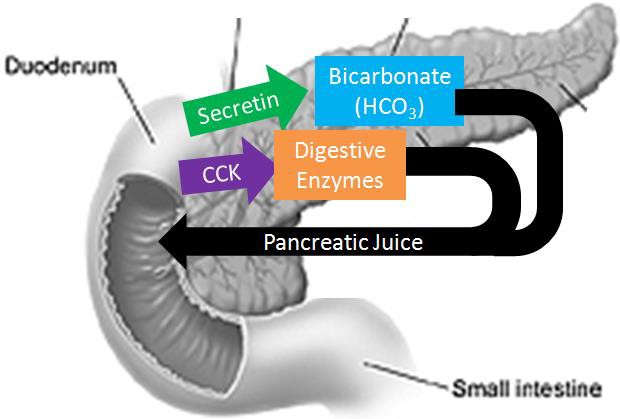
In addition, CCK also stimulates the contraction of the gallbladder causing the secretion of stored bile into the duodenum.
Pancreas
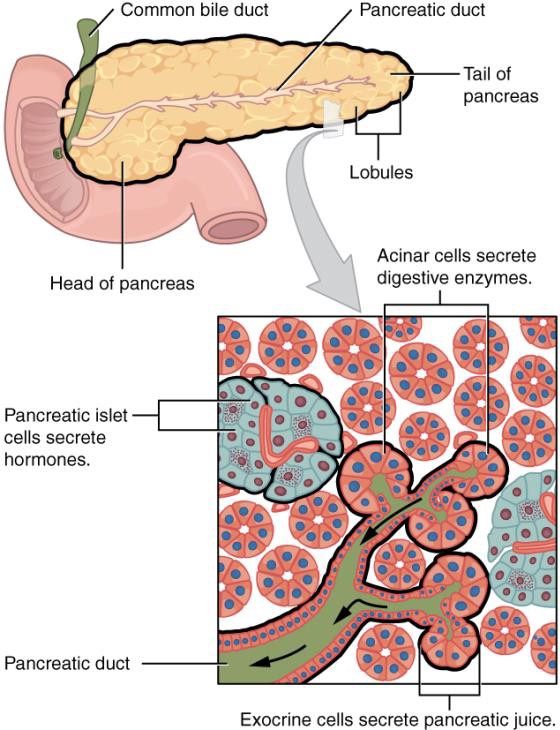
The pancreas is found behind the stomach and just above the transverse colon (part of the large intestine discussed later in this chapter). It is a tadpole-shaped organ consisting of a head, body, and tail. It is a unique organ containing both endocrine and exocrine portions. The smaller, endocrine (hormone-producing) portions contain alpha, beta, delta, and PP cells that secrete the hormones glucagon, insulin, somatostatin, and pancreatic polypeptide respectively. These cells are clustered in groups known as pancreatic islets (traditionally referred to as the Islets of Langerhans). However, the vast majority of the pancreas is made up of grape-like clusters of exocrine cells known as acini (singular = acinus). The cells composing each acinus are known as acinar cells. These acinar cells are responsible for producing enzyme-rich pancreatic juice. Pancreatic juice is released into small ducts that continually merge to form a large main pancreatic duct which delivers pancreatic juice from the pancreas to the duodenum, merging with the common bile duct (from the liver & gallbladder) along the way. The release of pancreatic juice, and bile, is controlled by the hepatopancreatic sphincter. The following video does a nice job of showing and explaining the function of the different pancreatic cells.
Video Link: The Pancreas Watch the first 53 seconds.
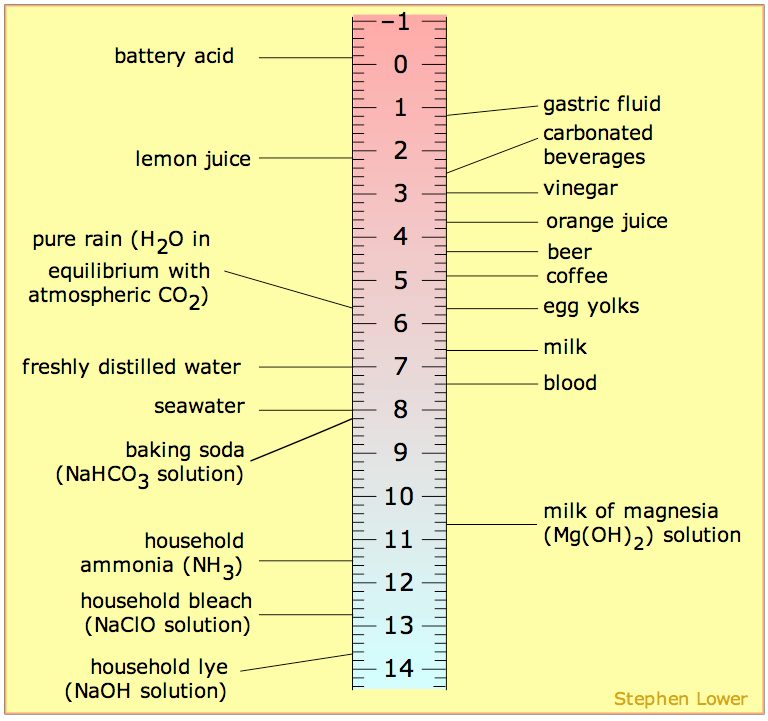
In addition to pancreatic hormones and enzymes, the pancreas releases bicarbonate. Bicarbonate is a base (high pH) meaning that it can help neutralize an acid (such as gastric juice.) You can find sodium bicarbonate (NaHCO3, baking soda) on the ruler below to get an idea of its pH.
The main digestive enzymes in pancreatic juice are listed in the table below.
Table 3.71 Enzymes in pancreatic juice
|
Enzyme |
Macronutrients Digested |
|
Pancreatic amylase |
Carbohydrates |
|
Proteases |
Protein |
|
Pancreatic Lipase |
Lipids |
|
Phospholipase A2 |
Lipids |
|
Cholesterol Esterase |
Lipids |
Liver
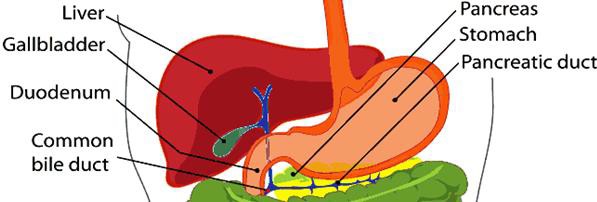
The liver is the largest internal, and the most metabolically active, organ in the body. The figure below shows the liver and the other accessory organs position relative to the stomach.
The liver is made up two major types of cells. The primary liver cells are hepatocytes, which carry out most of the liver’s functions. Hepatic is another term for liver. For example, if you are going to refer to liver concentrations of a certain nutrient, these are often reported as hepatic concentrations. The other major cell type is the hepatic stellate (also known as Ito) cells. These are fat storing cells in the liver.
The liver’s major role in digestion is to produce bile. This is a greenish-yellow fluid that is composed primarily of bile acids, but also contains cholesterol, phospholipids, and the pigments bilirubin and biliverdin. Bile acids are synthesized from cholesterol. The two primary bile acids are chenodeoxycholic acid and cholic acid. In the same way that fatty acids are found in the form of salts, these bile acids can also be found as salts. Because of this, these bile salts are often seen in texts with an (-ate) ending (chenodeoxycholate and cholate) indicating they are in the salt form.
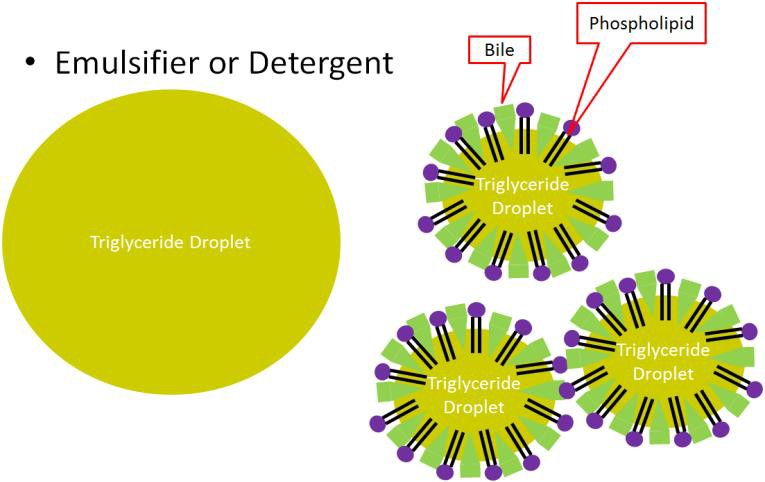
Bile acids, much like phospholipids, have both hydrophobic and hydrophilic portions. This makes them excellent emulsifiers that are instrumental in fat digestion. Bile is then transported to the gallbladder.
Gallbladder
The gallbladder is a small, sac-like organ found just off the liver (see Figure 3.74 above). Its primary function is to store and concentrate bile made by the liver. The bile is then transported to the duodenum through the common bile duct.
Why do we need bile?
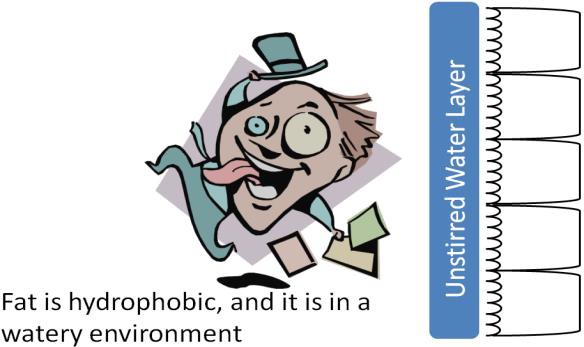
Bile is important because fat is hydrophobic, but the environment in the lumen of the small intestine is watery. In addition, there is an unstirred water layer that fat must cross to reach the enterocytes in order to be absorbed.
Triglycerides naturally form large triglyceride droplets to keep the interaction with the watery environment to a minimum. Picture the large droplets of cooking oil that form when you add it to water. This is inefficient for digestion, because enzymes cannot access the interior of the droplet. Bile acts as an emulsifier, or detergent. It, along with phospholipids, breaks the large triglyceride droplets into smaller triglyceride droplets that increase the surface area accessible for triglyceride digestive enzymes, as shown below.
Secretin and CCK also control the production and secretion of bile. Secretin stimulates the flow of bile from the liver to the gallbladder. CCK stimulates the gallbladder to contract, causing bile to be secreted into the duodenum, as shown in Figure 3.77.
Nutrients that are needed in large amounts and can be processed by the body into cellular energy - protein, fats and carbohydrates.
Accessory organs (salivary glands, liver, gallbladder, pancreas) do not come directly in contact with food or digestive contents, but still play a crucial role in the digestive process.
Duodenum is the first part of the small intestine.
Cholecystokinin (CCK) stimulates the secretion of digestive enzymes, also stimulates the contraction of the gallbladder causing the secretion of stored bile into the duodenum.
Tissues are groups of cells that share a common structure and function and work together.
Bile is produced in the liver and takes part in fat digestion. Bile acts as an emulsifier, or detergent. It, along with phospholipids, breaks the large triglyceride droplets into smaller triglyceride droplets that increase the surface area accessible for digestive enzymes.
Glucagon communicates to the cells in the body to stop using all the glucose. More specifically, it signals the liver to break down glycogen and release the stored glucose into the blood, so that glucose levels stay within the target range and all cells get the needed fuel to function properly.
Insulin is a hormone released from the pancreas that brings blood glucose levels down. Insulin sends a signal to the body’s cells to remove glucose from the blood by transporting it into different organ cells around the body and using it to make energy. In the case of muscle tissue and the liver, insulin sends the biological message to store glucose away as glycogen.
Phospholipids are molecules with two fatty acids and a phosphate group attached to a glycerol backbone. The fatty acids give a phospholipid a hydrophobic "tail" and the phosphate group gives the phospholipid a hydrophilic "head".
Emulsifiers can keep oil and water mixed. Emulsions are mixtures of two liquids that do not mix.
Enterocytes are the cells that line the villi of the small intestine and absorb nutrients. (also known as enteric cells or brush border cells).

