Chapter 4: Common Digestive Problems
4.7 Diverticulosis and Diverticulitis
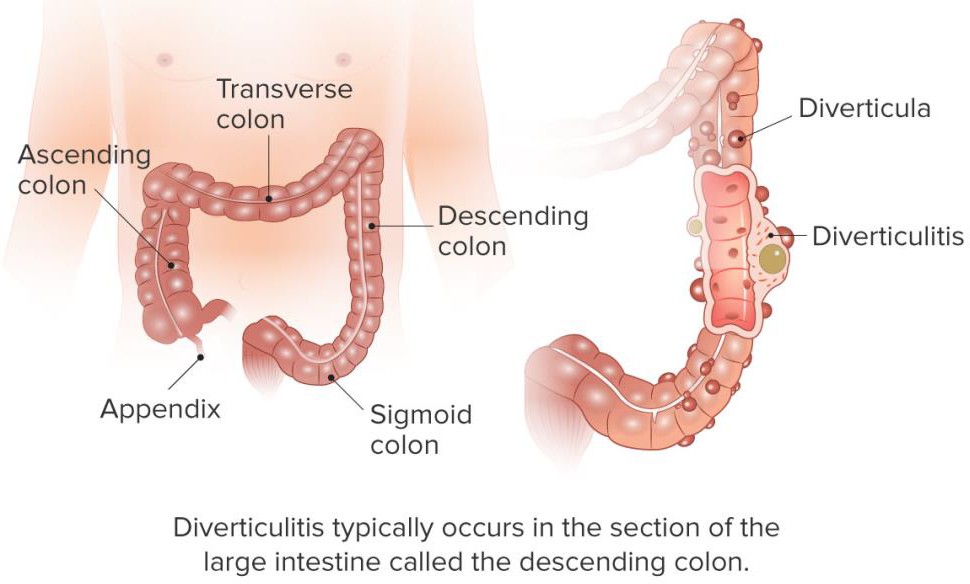
Approximately 10% of people under 40, and 50% of people over 60 years old have a condition known as diverticulosis.[1] In this condition, diverticula (plural, diverticulum singular), or out- pouches, are formed at weak points in the large intestine, primarily in the lowest section of the sigmoid colon, as nicely shown in the figure below and in the video in the web link below.
Video Link: Diverticulosis (1:24)
It is believed that diverticula are formed as a result of a low-fiber diet because people may strain more during bowel movements. Most people with diverticulosis do not know that they have the condition. However, if the pouches become inflamed, then the condition is known as diverticulitis. Approximately 10 to 25 percent of people who have diverticulosis go on to develop diverticulitis.[2] Symptoms include lower abdominal pain, nausea, and alternating between constipation and diarrhea.
The chances of developing diverticulosis and hence diverticulitis can be reduced with fiber intake because of what the breakdown products of the fiber do for the colon. The bacterial breakdown of fiber in the large intestine releases short-chain fatty acids. These molecules have been found to nourish colonic cells, inhibit colonic inflammation, and stimulate the immune system (thereby providing protection of the colon from harmful substances). Additionally, the bacterial indigestible fiber, mostly insoluble, increases stool bulk and softness increasing transit time in the large intestine and facilitating feces elimination. One uncomfortable side effect of consuming foods high in fiber is increased gas production since the byproducts of bacterial digestion of fiber are gases.
Several studies have found a link between high dietary-fiber intake and a decreased risk for colon cancer. However, an analysis of several studies published in the Journal of the American Medical Association in 2005 did not find that dietary-fiber intake was associated with a reduction in colon cancer risk.[3] There is some evidence that specific fiber types (such as inulin) may protect against colon cancer, but more studies are needed to conclusively determine how certain fiber types (and at what dose) inhibit colon cancer development.
The treatment the doctor prescribes will depend on how severe the condition is. Most cases of diverticulitis — about 75 percent of them — are uncomplicated. This means they have no other problems besides the actual inflammation or possible infection from the diverticulitis itself.
With uncomplicated diverticulitis, the doctor will likely suggest lots of rest and fluids during recovery from symptoms. They will also want to conduct follow-up assessments within a few days. In the meantime, the doctor may prescribe or recommend treatments such as medication, a liquid diet, or a low-fiber diet.[4]
- http://www.niddk.nih.gov/health-information/health-topics/digestive-diseases/diverticular-disease/Pages/facts.aspx#1 ↵
- National Digestive Diseases Information Clearinghouse, a service of National Institute of Diabetes and Digestive and Kidney Diseases, National Institute of Health. “Diverticulosis and Diverticulitis.” NIH Publication No. 08-1163 (July 2008). ↵
- Park, Y. et al. “Dietary Fiber Intake and Risk of Colorectal Cancer.” JAMA 294, no. 22 (2005): 2849–57. doi:10.1001/jama.294.22.2849 ↵
- https://www.healthline.com/health/diverticulitis#common-treatments ↵

